 While you may think that some tooth loss is inevitable with aging, it is actually possible for all of your teeth to last a lifetime. One way you can achieve this goal is to avoid Periodontal Gum Disease (“peri”—around; “odont”—tooth), which is caused by bacteria that attack the tissues around the teeth.
While you may think that some tooth loss is inevitable with aging, it is actually possible for all of your teeth to last a lifetime. One way you can achieve this goal is to avoid Periodontal Gum Disease (“peri”—around; “odont”—tooth), which is caused by bacteria that attack the tissues around the teeth.
Unfortunately, you may not even realize you have gum disease, as the signs and symptoms are not always as apparent to you as they are to a dental professional.
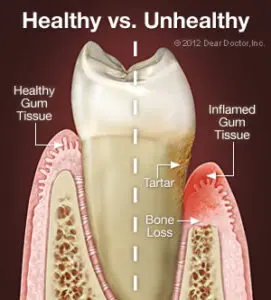
Nearly all people who do not maintain good daily oral hygiene will develop gingivitis. If left untreated, this bacterial gum infection can progress from gingivitis (“gingival” – gum; “itis” – inflammation) to periodontitis, which results in bone loss around your teeth.
As bone tissue is lost, the gum tissues detach from the teeth and form little pockets that provide a better place for bacteria to live—where your brush and floss can’t reach. As periodontal disease advances, tooth loss can result in more bone loss.
Part of this concerns genetics, as periodontal disease runs in families. The good news is that periodontal disease can be controlled, even at more advanced stages.
Signs and Symptoms of Periodontal Gum Disease
It’s important to understand that you can have periodontal disease with no obvious symptoms, especially if you are a smoker (nicotine reduces blood supply, preventing bleeding and swelling of the gum tissues). Still, there are some important things to look for:
- Bleeding gums — Some people think that when their gums bleed, it simply means they’re brushing too hard. While brushing too hard is bad for the gums, it should not cause bleeding. Any bleeding of the gums should be considered a warning sign of gum disease.
- Bad breath — It’s very easy for plaque to collect in the spaces between the teeth, creating the perfect living conditions for bacteria that produce odorous, sulfur-containing compounds, resulting in bad breath.
- Redness or swelling of the gums — Inflammation is usually the first visible sign of Periodontal Gum Disease.
- Receding gums — If you notice that your teeth look longer than they used to, it may be that your gum tissue has receded (away from the enamel), exposing some of your tooth roots.
- Sensitivity — If there is gum recession, the exposed roots may become sensitive to hot or cold.
- Periodontal abscess: Bacteria can become enclosed in a periodontal pocket and fill it with pus, causing it to become swollen and painful.
- Loose teeth — When periodontal disease results in bone loss, teeth can become loose or migrate. Tooth loss can result and may be accelerated if you are applying excessive biting forces from clenching or grinding your teeth.
Treatment Options
All periodontal therapy starts with an evaluation of your oral hygiene techniques and instructions for improving them. Then, plaque and any calcified deposits (tartar or calculus) present on the root surfaces are mechanically removed.
This is accomplished with a cleaning technique known as scaling, root planing, or debridement using hand instruments and/or ultrasonic (high-frequency vibrational) instruments.
Locally applied antimicrobial products or antibiotics might also be recommended during periodontal treatment to assist in healing and pocket-depth reduction, hopefully eliminating the need for periodontal surgery. Sometimes, surgical procedures may be necessary to remove the deep pockets between inflamed gum tissue and teeth.
There are many different types of surgery to handle a variety of problems. Many times, combinations of procedures are used to attempt to reduce the number of surgeries and the cost of treatment.
Periodontal Gum Disease & Your Overall Health
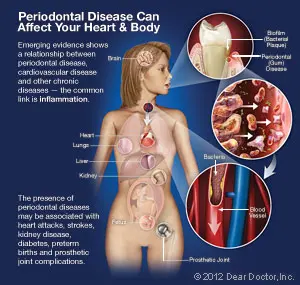
Periodontal gum disease starts in your mouth but has been linked to more severe conditions, such as cardiovascular disease (CVD), diabetes, and preterm births. Research has suggested two plausible mechanisms for how gum disease and these other serious medical concerns could be related: moderate to severe periodontal disease increases systemic (bodily) inflammation — a characteristic of all chronic inflammatory diseases.
Also, the same bacterial strains commonly found in periodontal pockets surrounding diseased teeth have been found in blood vessel plaques of individuals with CVD. Therefore, reducing periodontal inflammation may be helpful in reducing systemic inflammation.
Preventive Strategies For Periodontal Gum Disease
The best way to prevent periodontal disease is to brush and floss your teeth effectively daily.
Regular dental checkups and Professional Teeth Cleanings every 3 or 4 or 6 months are also crucial in maintaining periodontal health; the instruments and techniques used in these cleanings can reach into areas that your toothbrush and floss can’t.
It is also possible to detect early forms of gum disease by visually evaluating your gingival (gum) tissues and examining their attachment levels to the teeth.
Dental radiographs (X-ray pictures) can assess the health of your tooth-supporting bone.
Other steps you can take: Eating right, reducing stress, and giving up unhealthy habits like smoking will also help ensure that you keep your teeth for a lifetime.
What are the consequences of bone loss, gum recession, and periodontal disease?
Bone loss gum recession periodontal disease has significant implications for oral health. Periodontal disease causes inflammation of the gums and subsequent bone loss around teeth, leading to gum recession.
This exposes more of the tooth’s root, making it vulnerable to decay and sensitivity. The weakening of supporting structures can exacerbate bone loss. Effective prevention and treatment strategies are essential to mitigate these risks.
Bone loss, gum recession, periodontal disease, and periodontal disease gum surgery collectively impact oral health. Periodontal disease inflames gums and induces bone loss, leading to recession.
This exposes tooth roots, increasing decay risk. Weakened support structures exacerbate bone loss. Periodontal gum disease surgery aims to restore gum health and halt progression.
However, proactive prevention is optimal. Maintain oral hygiene, attend check-ups, and treat periodontal disease promptly. Lifestyle factors like smoking also contribute, so quit smoking and maintain a balanced diet. Implementing these measures can help safeguard against these oral health challenges.